Background
The National Leprosy Control Programme (NLCP) was launched by the GOI in 1955 with the primary aim of controlling leprosy through early detection and treatment, initially using Dapsone monotherapy.In the early 1980s, the World Health Organization (WHO) recommended Multi-Drug Therapy (MDT) as a game-changer in leprosy treatment. Responding to this, India restructured NLCP into the National Leprosy Eradication Programme(NLEP) in 1983, shifting the focus from control to elimination. MDT was introduced nationwide, and the programme adopted strategies to reduce transmission by detecting and treating all cases promptly. With World Bank assistance, NLEP was expanded to all districts by 1993–94, and in line with the National Health Policy 2002, India set a national goal to eliminate leprosy as a public health problem (defined as less than 1 case per 10,000 populations). This goal was successfully achieved at the national level in December 2005. Post-elimination, NLEP has focused on sustaining low prevalence, early case detection, reducing Grade II disabilities, and minimizing stigma through community engagement. Services have been integrated into the general healthcare system, supported by training and research institutes such as the Central Leprosy Teaching and Research Institute (CLTRI), Chengalpattu, and Regional Leprosy Training and Research Institutes (RLTRIs) in Raipur, Gauripur, and Aska.. The programme also emphasizes the role of Accredited Social Health Activists (ASHAs), household contact surveys, and use of digital platforms like Nikusth for case tracking. NLEP continues to work toward a leprosy-free India by sustaining elimination status, promoting rehabilitation, and eliminating discrimination against persons affected by leprosy
Overview of NLEP
The National Leprosy Eradication Programme (NLEP) is a centrally sponsored scheme functioning under the umbrella of the National Health Mission (NHM). The programme offers free-of-cost services for prevention, diagnosis, treatment, and rehabilitation of leprosy through all public health facilities across India. Its goal is to make India leprosy-free by interrupting transmission, eliminating stigma, and ensuring dignified care for all affected individuals.
NLEP provides both technical and financial support to all States and Union Territories for implementation of activities related to prevention, early detection, case confirmation, treatment, disability prevention, and post-treatment care. It also facilitates convergence with other national health programmes and deploys digital platforms such as Nikusth 2.0 for surveillance and reporting. The programme is aligned with the Sustainable Development Goals (SDGs) and the WHO Global Leprosy Strategy, aiming to achieve zero transmission, zero disability, and zero discrimination by 2027.
Vision
“Leprosy-free India” is the vision of the NLEP.
Mission
The NLEP’s mission is to provide quality leprosy services free of cost to all sections of the population, with easy accessibility, through the integrated healthcare system, including care for disability after cure of the disease.
Objectives:
- To reduce Prevalence rate less than 1/10,000 population at sub national and district level.
- To reduce Grade II disability % < 1 among new cases at National level.
- To reduce Grade II disability cases < 1 case per million populations at National level.
- Zero disabilities among new Child cases.
- Zero stigma and discrimination against persons affected by leprosy.
Strategy:
To achieve the aforementioned objectives, the main strategies to be followed are:
- To reduce Prevalence rate less than 1/10,000 population at sub national and district level.
- Early detection and complete treatment of new leprosy cases.
- Carrying out household contact surveys involving Accredited Social Health Activist (ASHA) in the early detection and completion of treatment of Leprosy cases on time.
- Strengthening of Disability Prevention and Medical Rehabilitation (DPMR) services.
- Information, Education and Communication (IEC) activities in the community to improve self-reporting to the Primary Health Centre (PHC) and reduce stigma.
- Intensive monitoring and supervision at Health and Wellness Centers and Block Primary Health Centre/Community Health Centre.
The following are the programme components:
- Case Detection and Management
- Disability Prevention and Medical Rehabilitation (DPMR).
- Information, Education and Communication (IEC), including Behaviour Change
- Communication (BCC)
- Human Resources and Capacity Building
- Programme Management
Milestones of NLEP:
| Year | Milestone |
|---|---|
| 1948 | Hind Kusht Nivaran Sangh |
| 1955 | National Leprosy Control Programme |
| 1983 | National Leprosy Eradication Programme started, MDT introduced |
| 1991 | World Health Assembly resolution to eradicate leprosy by 2000 AD |
| 1993 | World Bank supports the MDT programme – NLEP phase I |
| 2001-2004 | NLEP Project Phase II |
| 2002 | Simplified Information System Introduced |
| 2004 | Leprosy was integrated into the Integrated Disease Surveillance Programme (IDSP) |
| 2005 | National-level elimination achieved |
| 2005 | NLEP services integrated under National Rural Health Mission |
| 2007 | Disability Prevention & Medical Rehabilitation Guidelines introduced |
| 2014 | Upgraded Simplified Information System Implementation |
| 2016 | Rights of Persons with Disabilities Act |
| 2016 | Introduction of NIKUSTH - A real-time leprosy reporting software across India |
| 2017 | "Sparsh Leprosy Awareness Campaign" was launched |
| 2017 | PEP introduced to prevent leprosy using single-dose Rifampicin for contacts |
| 2019 | Leprosy screening converged with Ayushman Bharat - Comprehensive Primary Health Care |
| 2020 | Convergence of NLEP with Rashtriya Kishore Swasthya Karyakaram (RKSK) |
| 2021 | District award guidelines (August 2021) |
| 2023 | Revised classification of Leprosy & treatment regimen for PB & MB Cases in India |
| 2023 | Nukusht 2.0 launched |
| 2023 | AMR guideline and National Strategic Plan and roadmap (2023–27) launched |
| 2025 | Revised treatment implemented across India |
| 2025 | Leprosy declared a Notifiable Disease |
National Strategic Plan (NSP) 2023 – 2027
The National Strategic Plan and Roadmap for Leprosy 2023–2027 serves as India’s forward looking framework to achieve interruption of leprosy transmission at the district level by 2027. Developed in consultation with national experts, WHO, and key stakeholders, the plan aligns with the WHO Global Leprosy Strategy 2021–2030 and reflects India’s commitment to the Sustainable Development Goals (SDGs). The NSP promotes a patient-centric, rights-based approach to leprosy control and elimination. It is anchored on five strategic pillars:
- Leadership, Coordination, and Partnerships: Focuses on strengthening political commitment, inter-sectoral collaboration, and accountability at national, state, and district levels to ensure cohesive programme implementation.
- Accelerated Case Detection: Emphasizes proactive case finding through Active Case Detection Campaigns (ACDC), contact tracing, Focused Leprosy Campaigns (FLC), and integration with other health programmes to identify cases early and interrupt transmission.
- Comprehensive, Quality Leprosy Services: Ensures universal access to free diagnosis, treatment (MDT), disability care, reconstructive surgery, counseling, and post-treatment support through the general health system.
- Prevention of Disease, Disabilities, and Discrimination: Aims to prevent Grade II disabilities and reduce stigma through Post-Exposure Prophylaxis (PEP), disability prevention strategies, community engagement, and behavioral change communication.
- Robust Surveillance and Health Information Systems: Strengthens digital platforms like Nikusth 2.0, enables real-time case tracking, and supports data-driven planning, monitoring, and reporting across all administrative levels.
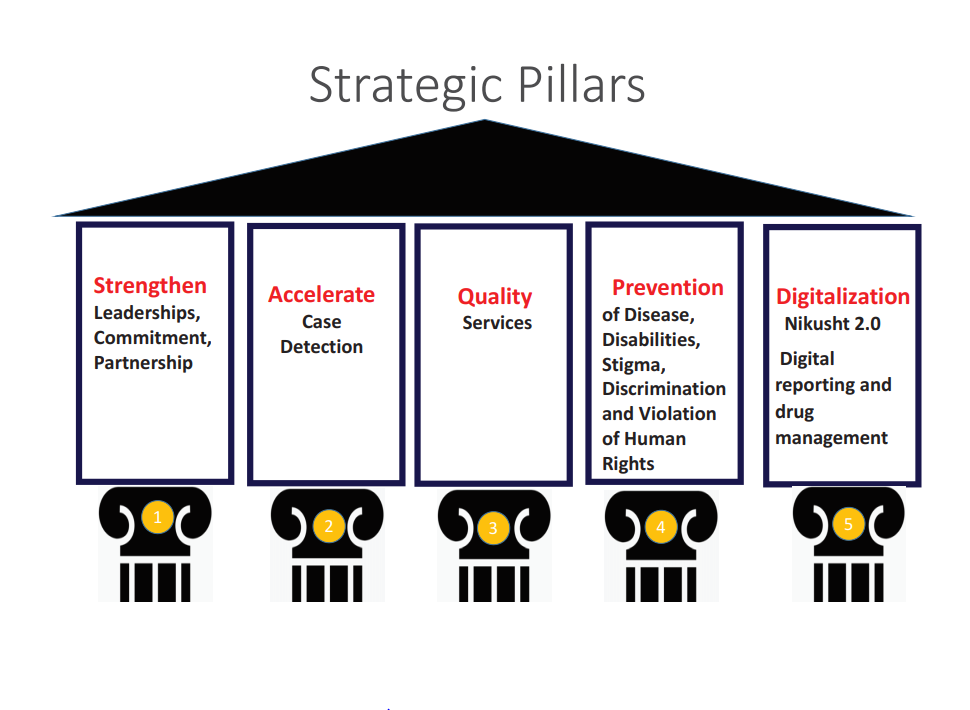
This strategic plan focuses not only on medical management but also on addressing social determinants, ensuring that persons affected by leprosy receive holistic care, protection, and dignity.
Antimicrobial Resistance (AMR) in Leprosy:
To address the growing concern of antimicrobial resistance (AMR) in Mycobacterium leprae, the Government of India has introduced dedicated AMR Guidelines under the National Leprosy Eradication Programme (NLEP). A national AMR surveillance network has been established across key institutions, including the Central Leprosy Teaching and Research Institute (CLTRI), Chengalpattu, Tamil Nadu, Schieffelin Institutes of health research, Karigiri, Tamil Nadu, LEPRA Blue Peter Public Health and Research Centre, Telangana, Stanley Browne Lab, Leprosy Hospital, TLM, Shahdara, Delhi, Regional Leprosy Training and Research Institute (RLTRI) Raipur, Chhattisgarh. These centers serve as sentinel sites to monitor resistance trends to key Multi-Drug Therapy (MDT) drugs—rifampicin, dapsone, and clofazimine. The initiative focuses on early detection, tailored treatment for resistant cases, and evidence-based policy refinement. This strategic response is pivotal for safeguarding MDT efficacy, ensuring uninterrupted care, and achieving the goal of zero leprosy transmission by 2027.

Activities under NLEP
- Diagnosis and treatment of leprosy- Free of cost Services for diagnosis and treatment (MDT) are provided by all public health care facilities including PHCs, CHC, DH, and Medical colleges throughout the country. Difficult to diagnose, complicated cases, reaction cases, and G2D cases requiring reconstructive surgery (RCS) are referred to the district hospital for further management.
- Revised Classification and Treatment Protocol (Effective April 1, 2025) - In 2023, India revised the classification and treatment protocols for leprosy in alignment with WHO recommendations. The updated protocol has been officially implemented nationwide from April 1, 2025. A 3-drug MDT regimen (Rifampicin, Dapsone, and Clofazimine) is now used for both PB and MB cases, enhancing uniformity and operational efficiency across public health facilities. The revised classification also emphasizes early detection based on lesion count and nerve involvement to minimize delays in treatment initiation.
- Capacity building- Training of general health staff like Medical Officers, health workers, health supervisors, laboratory technicians, and ASHAs is conducted every year to develop adequate skills for diagnosis and management of leprosy cases.
- IEC and counselling - Intensive IEC activities are conducted to generate awareness, which will help in the reduction of stigma and discrimination associated with persons affected by leprosy. These activities are carried out through mass media, outdoor media, rural media, and advocacy meetings. Major focus is also given on interpersonal communication.
- Disability Prevention and Medical Rehabilitation(DPMR) –For the prevention and management of disability, dressing material, supportive medicines, and micro-cellular rubber (MCR) footwear are provided to leprosy patients. The patients are also empowered with training in self-care procedures for preventing aggravating disability to the insensitive hands/feet. Emphasis is also being placed on correction of permanent disability through reconstructive surgeries (RCS). To strengthen. The patients concerned are provided RCS facility not only free of cost, but are also paid welfare allowances.
- Supervision and Monitoring –Programme is being monitored at different levels through analysis of monthly progress reports, through field visits by the supervisory officers, and programme review meetings held at central, state, and district levels. For better epidemiological analysis of the disease situation, emphasis is put on assessment of New Case Detection and Treatment Completion Rate and proportion of grade II disability among new cases. Visits by Joint monitoring Teams with members from the GOI, ILEP, and WHO have been an integral part of NLEP.
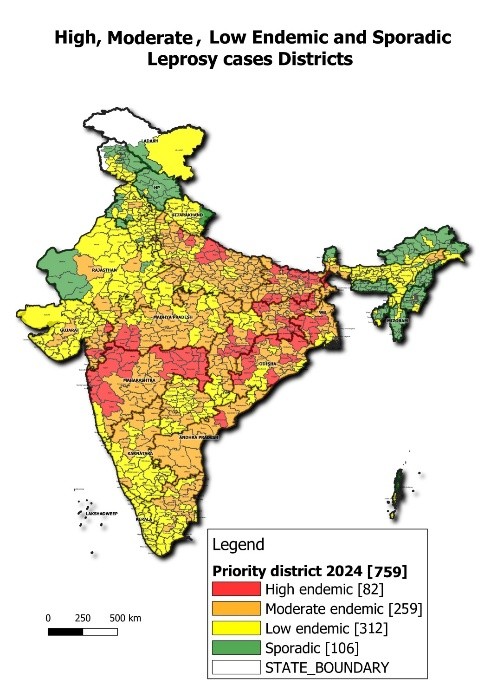
- District-level Elimination Achieved Nationwide: The number of districts reporting a prevalence rate of less than 1 case per 10,000 population increased from 542 in 2014–15 to 638 in 2024–25, indicating the achievement of leprosy elimination at the district level nationwide.
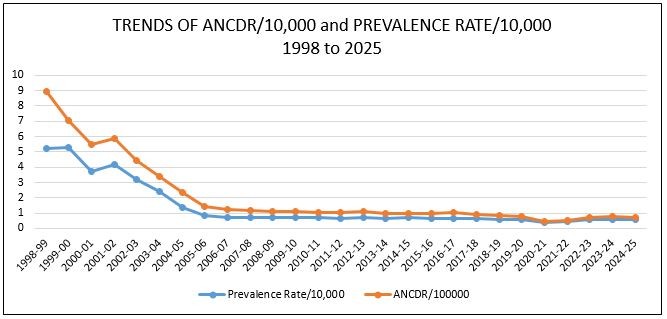
- Steady Decline in Prevalence Rate (PR): The national prevalence rate has decreased from 0.69 (2014–15) to 0.62 (2018–19) and further to 0.57 (2024–25), reflecting enhanced early detection and effective treatment coverage.
- Reduction in Grade 2 Disability (G2D): G2D among new cases—a key indicator of delayed diagnosis—has significantly dropped from 4.48 per million population in 2014–15 to 1.31 in 2024–25, highlighting improved case finding and early intervention.
- Lower Proportion of Child Cases: The percentage of children among newly detected cases has declined from 9.04% in 2014–15 to 4.68% in 2024–25, indicating reduced community transmission and timely identification.
- Decline in Annual New Case Detection Rate (ANCDR): The number of new leprosy cases detected annually reduced from 100,957 in 2024–25, corresponding to an ANCDR of 7.00 per 100,000 populations, down from 8.69 in 2018–19 and 9.73 in 2014–15.
- Leprosy Case Detection Campaign (14 days) in high endemic districts.
- Focused Leprosy Campaign (FLC) in low endemic districts for case detection.
- Special plans for Hard-to-Reach areas for early case detection and treatment.
- ASHA Based Surveillance for Leprosy Suspects (ABSULS)- in low endemic districts Focused Leprosy Campaign (FLC) in low endemic districts.
- Monitoring and Supervision - Regular national, state, and district-level review meetings and field visits are conducted to ensure programme performance, data quality, and treatment outcomes.
- Convergence of leprosy screening under NHM: Convergence of leprosy screening for targeting different age groups like under RBSK (for 0-18 yrs), RKSK (13-19 yrs), and CPHC – Ayushman Bharat (above 30+ yrs population).
- Timely referral and follow up for treatment completion on time through Multi Drug Therapy (MDT) available free of cost in all public health facilities.
- For prevention of leprosy amongst contacts: Post Exposure chemoprophylaxis administration (PEP) with Single dose of Rifampicin (SDR) given to the eligible contacts of index case in order to interrupt the chain of transmission.
- Reconstructive Surgeries (RCS) are conducted at District Hospitals/Medical Colleges/ Central Leprosy Institutes, and welfare allowance @ Rs 12,000/- is paid to each patient undergoing RCS.
- IEC & Training : Routine IEC activities are conducted by states and districts throughout the year, Special Annual Mass Awareness campaigns named Sparsh Leprosy Awareness Campaigns (SLAC) were launched on 30th January, 2017 i.e., Anti Leprosy Day, to reduce stigma and discrimination against persons suffering from leprosy. Since then every year, nationwide Gram Sabhas in villages across the country are being organised in cooperation and coordination with allied sectors of health department. Appropriate messages from District Magistrates and appeals from Gram Sabha Pramukh (Heads of Village councils) to reduce discrimination against persons affected with leprosy are read out; pledge is taken by all Gram Sabha members to reduce the burden of disease in the community, and felicitation of persons affected with leprosy is done. Village community is encouraged to participate in these meetings, and school children are encouraged to spread awareness about the disease through plays, posters etc.
| Revised classification of leprosy | ||||
|---|---|---|---|---|
| S. No. | Types | Skin lesions | Nerve Involvement | Bacilli in laboratory-based test (Slit Skin Smear) |
| 1 | Pauci-Bacillary (PB) | 1–5 | No nerve (0) | Absent (Negative) |
| 2 | Multi-Bacillary (MB) | More than 5 (>5) | One or more nerve involved (≥ 1) | Present (Positive) |
| Revised treatment Regimen | ||||||
|---|---|---|---|---|---|---|
| S. No. | Types | Duration of treatment | Dapsone | Clofazimine | Rifampicin | |
| 1 | Pauci-Bacillary | Adult - 6 months | 100 mg Daily | 300 mg once a month & 50 mg daily | 600 mg once a month | |
| Child (10-14 years) - 6 months | 50 mg Daily | 150 mg once a month & 50 mg alternate day | 450 mg once a month | |||
| Child <10 years or <40kg (20–40kg) - 6 months | 2 mg/kg daily | 100 mg once a month, 50 mg twice weekly | 10 mg/kg once a month | |||
| 2 | Multi-Bacillary (MB) | Adult - 12 months | 100 mg Daily | 300 mg once a month & 50 mg daily | 600 mg once a month | |
| Child (10-14 years) - 12 months | 50 mg Daily | 150 mg once a month & 50 mg alternate day | 450 mg once a month | |||
| Child <10 years or <40kg (20–40kg) - 12 months | 2 mg/kg daily | 100 mg once a month, 50 mg twice weekly | 10 mg/kg once a month | |||
Note: *The treatment for children with body weight below 40 kg requires single formulation medications since no MDT combination blister packs are available.# For children between 20 and 40 kg, it would be possible to follow the instructions of the Operational Manual, Global Leprosy Strategy 2016–2020 on how to partly use (MB-Child) blister packs for treatment
Major achievements under the National Leprosy Eradication Programme (NLEP) during the last 10 years (2015-2025) with respect to March’2014 are as follows:
Major Indicator-wise, achievements are as under:
| Indicators | 2014-15 | 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 | 2020-21 | 2021-22 | 2022-23 | 2023-24 | 2024-25 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence Rate | 0.69 | 0.66 | 0.66 | 0.67 | 0.62 | 0.57 | 0.40 | 0.45 | 0.57 | 0.60 | 0.57 |
| Percentage of Child Cases | 9.04 | 8.94 | 8.69 | 8.15 | 7.67 | 6.87 | 5.76 | 5.45 | 5.38 | 5.18 | 4.68 |
| Grade 2 Disability per Million | 4.48 | 4.46 | 3.89 | 3.34 | 2.65 | 1.96 | 1.10 | 1.36 | 1.69 | 1.63 | 1.31 |
| Annual New Case Detection Rate / 100000 | 9.73 | 9.71 | 10.17 | 9.27 | 8.69 | 8.13 | 4.56 | 5.52 | 7.44 | 7.55 | 7.00 |
Projections for NLEP targets under National Strategic Plan (NSP) and Roadmap for Leprosy 2023-27:
| Indicators | 2022-23 | 2023-24 | 2024-25 | 2025-26 | 2026-27 |
|---|---|---|---|---|---|
| New Leprosy Cases | 115000 | 110000 | 80000 | 65000 | 50000 |
| Child Cases | 6000 | 5000 | 4000 | 2000 | 1000 |
| Child Percentage | 5.21 | 4.5 | 5 | 3.07 | 2 |
| Grade 2 Disability per Million | 1.7 | 1.8 | 1.2 | 1 | 0.5 |
District endemicity:
Highest Priority (High Endemic), High Priority (Moderate endemic)
Key Initiatives:
The Theme for the year 2025-26 for SLAC is "Together, let us raise awareness, dispel misconceptions and ensure that no one affected by leprosy is left behind".

“Sapna” is a concept (mascot) designed and developed using a common girl living in community, who will help spread awareness in the community, through key IEC messages. Sapna can be local school going girl who is willing to be ‘Sapna’. There can be any number of Sapnas in a village.
NLEP Directory
Last Updated On 19/06/2025